Learning Objectives
By the end of this topic, the student should be able to:
- Describe the medical indications for the short-term use of opioids.
- Describe the medical indications where opioids are used for longer periods of time.
- Identify the reasons for the non-medical use of opioids.
- Differentiate between acute and chronic adverse effects of opioids.
- Discuss how opioid use can result in tolerance, dependence, and opioid use disorder.
- Describe the impact of opioid use on others, including family members.
Key Concepts
- Opioids are used to treat acute pain.
- Opioids are used to treat chronic cancer pain and sometimes other types of chronic pain.
- Opioids are also used for recreational purposes, for self-medication, and to treat symptoms of opioid withdrawal.
- Opioids cause adverse effects, including sedation, nausea, constipation, itchy skin, and several others.
- Opioids also cause adverse effects when used over long periods, including sleep disturbances and hormonal changes.
- Continued use of opioids can result in tolerance. A person may need to use an increasing amount of an opioid to obtain the same effect.
- Continued use of opioids can result in dependence. An opioid-dependent person will experience symptoms of withdrawal if opioids are stopped abruptly.
- Opioid use disorder is officially diagnosed based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria.
- The effect of opioid use on families can vary depending on the type of family structure.
Short-Term Opioid Use
Opioids are used primarily for their pain-relieving (analgesic) effects for moderate to severe acute pain due to a variety of causes.

Opioids affect pain in several ways:
- Normally, pain is signaled to the brain via activation of the ascending pain pathway. The ascending pain pathway delivers the pain signal from the source of the pain to the brain via the spinal cord. Opioids inhibit this pain transmission signal.
- Opioids also increase the activity of the descending inhibitory pathway. This pathway works from the brain down to the spinal cord, so works in the opposite direction of the ascending pain pathway. The pathway inhibits the ascending pain signal, so further reduces pain.
- Finally, opioids decrease the subjective perception of pain (i.e., increased pain tolerance)
Less commonly, opioids are used to suppress severe cough and to treat diarrhea. Opioids are also used in combination with other drugs in anaesthesia.
Opioids for short-term pain are usually recommended for a short period, like a few days or for few weeks. As the person recovers, the pain lessens each day and results in reduced need for opioids. However, even with short-term use, opioids may lead to physical dependence or addiction.
Long-Term Opioid Use
Although opioids are used to treat a wide variety of types of acute pain, their use and effectiveness for most types of chronic pain are controversial.

- Opioids are frequently used for chronic cancer pain.
- Opioids are sometimes used for chronic, non-cancer pain but are less effective than previously thought.
- Alternatives to opioids, such as non-opioid analgesics including acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) should be tried first, and antidepressants and anticonvulsants are preferred agents for chronic nerve pain.
- When opioids are used for chronic pain, best practices suggest keeping the daily doses below 90 MME (morphine equivalents), if possible, to frequently assess and reassess for effectiveness and adverse effects, and to avoid using other central nervous system depressants, particularly benzodiazepines.
Long-term opioid use is often linked to poor physical health or simultaneously using a benzodiazepine or a history of heroin use.
- The number of deaths from opioid overdose is higher in clients on long-term use of opioids.
- Long-term use of opioids can result in severe adverse effects on the respiratory, cardiovascular, immune, gastrointestinal, and central nervous system.
“Non-Medical” Use of Opioids
The use of opioids for reasons other than the treatment of pain as managed by a prescriber is sometimes called non-medical use; however, this description can be misunderstood.
Opioids can also be used for self-medication of:
- physical pain,
- emotional pain, and trauma,
- or to avoid symptoms of opioid withdrawal.
Although these are medical reasons, when used outside the medical system they are sometimes called non-medical use.
- This type of use is also sometimes called misuse or abuse.
Prescription and unregulated opioids can be used recreationally—for pleasure.
- In many cases, a combination of recreational and self-medication reasons may contribute to ongoing opioid use.
- Persons with opioid use disorder may feel compelled to keep using opioids or to use more opioids.
Adverse Effects of Opioids—Acute
Opioids have several adverse effects. These may vary between opioids and generally increase as the dose and frequency of use is increased:
- sedation, sleepiness, difficulty concentrating
- nausea and vomiting
- constipation
- urinary retention
- itchiness
- sweating
- respiratory depression
- sleep disturbances
- changes in mood including euphoria or dysphoria
Adverse Effects of Opioids—Chronic
Many of the acute adverse effects of opioids may persist when opioids are used over longer time periods; some may improve and some may worsen.
In addition, long-term opioid use can also result in the following:
- hormonal changes that can affect mood and sexual function or cause amenorrhea (women not having their period) and gynecomastia (breast enlargement)
- hyperalgesia (when opioids worsen pain instead of improving it)
- tolerance
- dependence
- addiction/use disorder
Tolerance
The human body has its own natural opioid system that works to regulate pain, mood, the GI tract, and many other functions.
Endogenous opioids are naturally occurring neuromodulators, produced and secreted by nerve cells. They are small peptides that include several types of endorphins, enkephalins, and dynorphins that bind and activate opioid receptors.
Like all systems in the body, the opioid system is constantly fine-tuned. If the system becomes over-activated, the body takes steps to reduce this activity, and if the system is downregulated, the body takes steps to increase activity.
Definition
- Exogenous Opioids
- Opioids from an external source rather than those the body produces itself.
When exogenous opioids are taken, the endogenous opioid system detects the over-activity they cause, and reacts by reducing activity. It does this by reducing production of endogenous opioid peptides and reducing the number of opioid receptors, among other things.
- At this stage, the body has begun to adapt to the presence of the exogenous opioid.
- As the body adapts, tolerance can occur: the person needs more and more of the drug to produce the same effect.
If opioid use is stopped, the opioid system returns back to its original state, but this can take several weeks to months depending on the individual.
Dependence and Withdrawal
With continued use, the body’s opioid system activity may be further and further impaired. Eventually, endogenous opioid system activity is reduced to the point that the body becomes reliant on continued exogenous opioids—termed opioid dependence.
Once a person is dependent on opioids, they will experience symptoms of opioid withdrawal if they stop taking opioids. How fast these withdrawal symptoms start depends on the half-life of the opioid used:
- muscle aches and weakness
- diarrhea and stomach cramps
- nausea and vomiting
- shivering/goose bumps
- yawning
- sweating, changes in body temperature
- anxiety
- restlessness
- sneezing and runny nose
- fast heart rate
- sleep disturbances
When these symptoms occur, they are readily reversed by additional doses of an opioid. Withdrawal symptoms can be minimized by tapering the dose of the opioid.
Withdrawal severity is assessed clinically using the Clinical Opiate Withdrawal Scale (COWS) (Wesson & Ling, 2003).
Opioid Use Disorder
Experiencing tolerance, dependence, or withdrawal on their own does not mean a person has opioid use disorder. The Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnosis can be mild (two to three symptoms), moderate (four to five symptoms), or severe (six or more symptoms).
A diagnosis of opioid use disorder is described in the DSM-5 (American Psychiatric Association, 2013). Two of the following must be observed within a 12-month period:
- Opioids are often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control opioid use.
- A great deal of time is spent in activities necessary to obtain the opioid, use the opioid, or recover from its effects.
- Craving, or a strong desire or urge to use opioids is present.
- Recurrent opioid use results in a failure to fulfill major role obligations at work, school, or home.
- Opioid use continues despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Important social, occupational, or recreational activities are given up or reduced because of opioid use.
- Recurrent opioid use occurs in situations in which it is physically hazardous.
- Opioid use continues despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
- The person exhibits tolerance.
- The person exhibits withdrawal, including self-medication to manage withdrawal.
For clients using prescription opioids, screening tools such as the Prescription Opioid Misuse Index (POMI) may be employed by physicians or health and social service professionals.
On a societal level, opioid use or opioid use disorder can increase the following:
- marginalization and loss of social cohesion
- family break down
- absenteeism from school and work
- criminal activity
Impact of Opioid Use on Families

There are various types of family structures: single parent, multigenerational, traditional nuclear families, foster families, and so on. The effect of opioid abuse on families will vary depending on the type of family structure.
- In a single-parent household, children may take the role of a surrogate spouse to support the parent who has an opioid use disorder.
- Extended family members may experience abandonment, anxiety, fear, anger, embarrassment, or guilt and may even wish to cut ties with the person with an opioid use disorder (Center for Substance Abuse Treatment, 2004).

A systematic review of the effects of opioid use on parent-child relationships found the following (Romanowicz, 2019):
- Studies on mother-child interaction found that mothers with opioid use disorders were more irritable, ambivalent, and disinterested while showing greater difficulty interpreting children’s cues compared with the control group.
- Children of a parent with opioid use disorder can display greater amounts of disorganized attachment, be less likely to seek contact, and be more avoidant than the control groups.
- “The children also had increased risk of emotional and behavioural issues, poor academic performance, and poor social skills”.
- Younger children had an increased risk of abuse or neglect and were more prone to later life issues such as unemployment, legal issues, and substance abuse.
- Consequences can arise even before birth. For example, opioid drug therapy during pregnancy may negatively affect the unborn child.
- This can result in neonatal abstinence syndrome (NAS), a condition linked to birth defects and severe withdrawal symptoms exhibited by the infant at birth.
- Symptoms of NAS can include irritability, crying, yawning, poor feeding, vomiting, diarrhea, and others.
Social workers suggest the following when working with an individual and their family:
- Consider the family from the client’s point of view (who does the client describe as their family member?).
- Assess the effectiveness of the family’s communication and their supportiveness or negativity, parenting skills, conflict management, and understanding of addiction.
- After a period of separation, family members are sometimes more willing to participate in the treatment process.
Family members may also need support to rebuild relationships with the person in treatment after a disruption in trust and communication caused by opioid use.
Take a moment to review the diagram adapted from The effects of prenatal opioid use on the parent-child relationship and children’s development and behavioural outcomes: a systematic review of published reports.
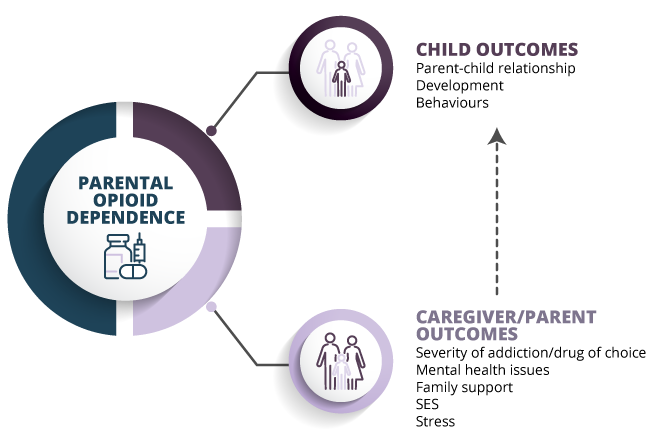
Adapted from (Romanowicz, 2019);
_human/iStock (template); Vladislav Popov/iStock (opioids); anttohoho/iStock (family)