Learning Objectives
By the end of this topic, the student should be able to:
- Describe how opportunities can be created to promote positive mental health.
- Describe ways that wellness and self-care can foster healing.
- Recognize how to promote resilience to improve health outcomes.
Key Concepts
- Wellness is an active process through which people become aware of, and make choices towards, a healthier lifestyle and greater overall well-being or existence.
- Wellness is a holistic concept and framework that is focused on achieving and maintaining balance in all aspects of life (e.g., mental, emotional, physical, spiritual, environmental, occupational, economic).
- Different cultures use different frameworks of wellness, which emphasizes the importance of listening to and respecting the values, beliefs, practices, and preferences of the client.
- Promoting change within systems of care and practices is needed to create space for diverse wellness frameworks and approaches, thereby reducing the health inequities of marginalized groups.
- Opioid misuse and addiction might be an attempt to cope with a past traumatic event.
- Creating resilience in communities helps to ensure people with substance use disorders have the resources and supports needed to equalize their opportunities for success.
What Does Wellness Mean?
Definition
- Wellness
-
- a conscious, self-directed, and evolving process of achieving full potential,
- multidimensional and holistic, encompassing lifestyle, mental and spiritual well-being, and the environment, and
- positive and affirming.
National Wellness Institute (Hettler, 1976)
Wellness means being mindful of different dimensions of life, which includes emotional, occupational, physical, social, intellectual, and spiritual aspects.
- Working toward all dimensions builds resiliency and positive coping skills.
Six Dimensions of Wellness

- Physical: A healthy body through exercise, nutrition, sleep, etc.
- Mental: Engagement with the world through learning, problem-solving, creativity, etc.
- Emotional: Being in touch with, aware of, accepting of, and able to express one’s feelings (and those of others).
- Spiritual: Our search for meaning and purpose in human existence.
- Social: Connecting with, interacting with, and contributing to other people and our communities.
- Environmental: A healthy physical environment free of hazards; awareness of the role we play in bettering rather than denigrating the natural environment.
(Global Wellness Institute, n.d.)
When working with someone who is healing from trauma or violence, it is important to support them in all aspects of their life, as reflected by the holistic model and examples listed below.
What opportunities for wellness can look like
How a person contributes to their environment and community, and how to build better living spaces and social networks.
The benefits of regular physical activity, healthy eating habits, expanding social networks, strength, and vitality.
The enrichment of life through work, and its interconnectedness to living and playing.
Self-esteem, improving social skills, self- control, and self-determination as a sense of direction.
The development of belief systems, values, and attitudes that result in the adoption of healthy living behaviours or actions.
Creative and stimulating mental activities, and sharing one’s gifts with others.
Ensuring organizational policies and practices focus on developing partnerships with communities to incorporate diverse perspectives and approaches to wellness within existing organizational structures, systems, and processes.x
Health care organizations and health and social service providers collaborate with communities to protect and strengthen traditional medicines and practices and promote their (culturally appropriate) inclusion and application within mainstream health care settings.
It is important to start where the individual is and listen to what they identify as helpful, as explained in this short YouTube video featuring Dr. Pat Ogden.
Listen to ways in which coping skills can be introduced (NICABM, 2014):

People with histories of trauma often struggle when accessing health care services and can find these services are re-traumatizing. Using a trauma- and violence- informed approach can help people to engage in more meaningful encounters with their providers and feel more comfortable in those encounters.
Wellness and Culture
It is important to be aware that different cultures have different understandings of wellness and not to impose one’s viewpoint or cultural perspective onto another person. For example, the concept of individual self-care is not necessarily viewed as a natural element in cultures that are collectivist as opposed to individualist.
Indigenous people might embrace a different path to wellness and health. Click to see an Indigenous wellness framework (PDF) created by Elder Jim Dumont (2015)
Mindfulness as a Coping Response
The study of mindfulness as a treatment for stress and chronic pain is more than 30 years old; however, it is not consistently recognized as a useful approach or coping mechanism in the field of substance use disorders.

olegbreslavtsev/iStock
Definition
- Mindfulness
- A moment-to-moment awareness of one’s experience without judgment. In this sense, mindfulness is a state and not a trait. While it might be promoted by certain practices or activities, such as meditation, it is not equivalent to or synonymous with them (Davis and Hayes 2012, p. 66).
Mindfulness involves meditative practices that foster “awareness that arises from paying attention, on purpose, in the present moment and non-judgmentally” (Kabat-Zinn, as cited in Purser, 2015). It is gaining legitimacy as a holistic approach to cope with anxiety, depression, and chronic pain—conditions that can lead to substance use.

- Research on the impacts of mindfulness practice on opioid use found that cravings and pain associated with opioid use can be reduced through the use of mindfulness techniques complimented by medication (i.e., methadone maintenance therapy).
- Mindfulness-based interventions also have been successfully used in conjunction with psychotherapy counselling approaches such as cognitive behavioural therapy to reduce cravings, anxiety, and stress, within people experiencing substance use disorders.
Mindfulness can be an effective tool to promote improved self-care and prevent and reduce compassion fatigue and burnout among health care and social service providers.
The image below outlines techniques used by the mindfulness approach and the relationship with biological and behavioural mechanisms, leading to resulting clinical outcomes.
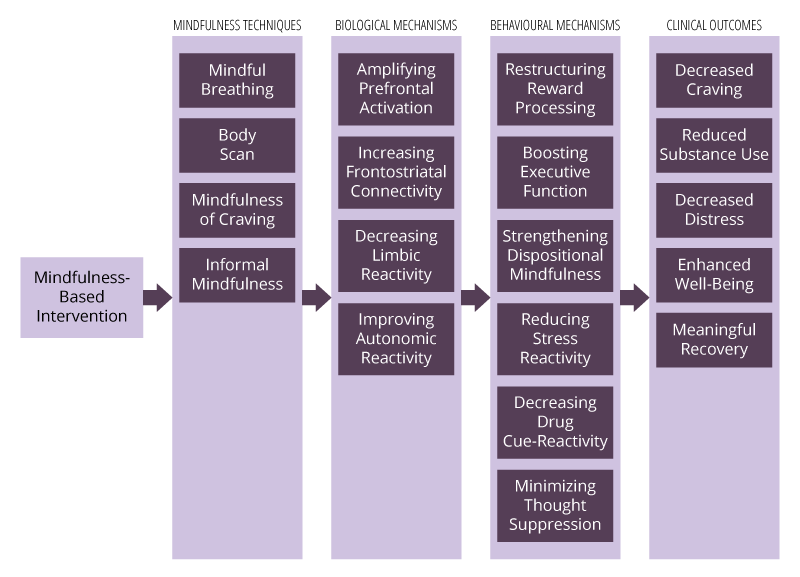
Mindfulness techniques such as mindful breathing, body scan, mindfulness of craving, and informal mindfulness are used in mindfulness based interventions. They are used in conjunction with biological mechanisms such as amplifying prefrontal activation, increasing frontostriatal connectivity, decreasing limbic reactivity, and improving autonomic reactivity, and behavioural mechanisms such as restructuring reward processing, boosting executive function, strengthening dispositional mindfulness, reducing stress reactivity, decreasing drug cue-reactivity, minimizing thought suppression. Resulting clinical outcomes include decreased craving, reduced substance use, decreased distress, enhanced well-being, meaningful recovery.
(Garland & Howard, 2018)
Opioid Use and Building Resilience
Problematic opioid use and addiction might be an attempt to cope with a past traumatic event. As confirmed by multiple research studies, opioid use and addiction are common responses to trauma. Health and social service providers should focus on strengths rather than deficits and provide opportunities for people to build skills (coping skills, self-regulation skills such as mindfulness, and recognition of triggers):
- Acknowledge the resilience of individuals who experienced trauma.
- Promote increasing social, emotional, and resiliency skills.
- Encourage grounding skills and coping skills for managing trauma (recognizing triggers, self de-escalating, centring, staying present-minded).
- Facilitate the development of pain management skills (through relaxation techniques, mindfulness, yoga, physical exercise, breathing techniques).
- Promote attachment and relational skills.
- Create safety plans and facilitate goal setting.
Creating resilience in communities also helps to ensure people with substance use disorders have equal opportunities to succeed:
- Social determinants of health (education, employment, housing, and income) are highly correlated with an individual’s sense of competence and control. These influence a person’s ability to cope and thrive within their environment.
- Housing with supports, including health services, income support, social support, and securing employment can immensely help individuals with substance use issues gain stability in their lives.
- Investing in community resources such as by enhancing community-based services and peer support services, and improving engagement with the primary care sector, can improve access to services and facilitate greater engagement with resources and supports, thereby reducing health inequalities and creating more resilient communities.

Support policies and regulations that promote health, affordable housing, accessible employment resources, and income support are essential.
Health and social service providers must work to change policies and practices that do not respond to diversity or that re-colonize, such as regulations (including funding structures, systems, or processes) that limit or prevent Indigenous communities from designing and governing health and social services that recognize and support prevention, access, and use of traditional medicines and land-based healing practices.
- A move to require agencies to have people with lived experience and family members as voting members on health and social service organization boards to develop inclusive community tools and resources is important.
- Health and social service providers should support the implementation of a shared and laddered care model.
Questions
References
Assembly of First Nations. (2015). First Nations mental wellness continuum framework. Health Canada. https://thunderbirdpf.org/first-nations-mental-wellness-continuum-framework/
Davis, D. M., & Hayes, J. A. (2012). What are the benefits of mindfulness? Monitor on Psychology, 43(7), 65–70. https://www.apa.org/education/ce/mindfulness-benefits.pdf
Dumont, J. (2014). Indigenous wellness framework. https://thunderbirdpf.org/wp-content/uploads/2015/07/4_Indigenous_Wellness_Framework.pdf
Garland, E. L., & Howard, M. O. (2018). Mindfulness-based treatment of addiction: current state of the field and envisioning the next wave of research. Addiction Science & Clinical Practice, 13(1), 14. https://doi.org/10.1186/s13722-018-0115-3
Global Wellness Institute. (n.d.). What is wellness? https://globalwellnessinstitute.org/what-is-wellness/
Hettler, B. (1976). Six dimensions of wellness model. National Wellness Institute. https://cdn.ymaws.com/members.nationalwellness.org/resource/resmgr/pdfs/sixdimensionsfactsheet.pdf
Kabat-Zinn, J., & Hanh, T. N. (2009). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Bantam Books.
Nathoo, T., Poole, N., & Schmidt, R. (2018). Trauma-informed practice and the opioid crisis: A discussion guide for health care and social service providers. BC Centre of Excellence for Women’s Health.
National Native Addictions Partnership Foundation. (2014). Honouring our strengths: Indigenous culture as intervention in addictions treatment project—University of Saskatchewan (Funding Reference Number AHI-120535). Canadian Institutes of Health Research.
NICABM. (2014, October 31). How to help trauma patients feel safe [Video]. YouTube. https://www.youtube.com/watch?v=-eQ64ctFUUk
Purser, R. (2015). The myth of the present moment. Mindfulness, 6, 680–686. https://doi.org/10.1007/s12671-014-0333-z
Taha, S., Maloney-Hall, B., & Buxton, J. (2019). Lessons learned from the opioid crisis across the pillars of the Canadian drugs and substances strategy. Substance Abuse Treatment, Prevention, and Policy, 14(1), 1–10.