Learning Objectives
By the end of this topic, the student should be able to:
- Discuss the need for a critical gender lens in screening, assessment, and intervention.
- Describe racial influences in drug use and stigmatization.
- Review the impact of colonialism on harmful opioid use.
- Define a decolonizing approach to care
Key Concepts
- Sex-related factors affect how the body reacts to substances: how substances are metabolized, what amount causes intoxication, their effects on the brain, and the development of tolerance, dependence, or a disorder. Female and male bodies have different genetic and physiological characteristics that affect these processes.
- Gender-related factors include the impacts of roles, norms, power imbalances, identity, and institutional gender on men, women, and gender-diverse individuals. These affect risks and/or opportunities for use, impact of and exposure to marketing or exploitation, access to care and services, pressures to use, and the societal response to problematic use.
- Women have higher rates of prescription opioid use and higher prevalence of pain disorders and depression and anxiety disorders, leading to prescription opioid misuse.
- Men use opioids at higher rates, in larger quantities, and with more overdose deaths, often dying alone or without accessing help.
- Black persons, Indigenous persons, and persons of colour experience more police attention, incarceration, cultural dislocation, trauma and damage, all of which affect substance use patterns.
- Indigenous persons in Canada experience intergenerational trauma as a direct result of colonialism
- It is critical to understand the impact and relationship between colonialism, racism and determinants of health and the risks opioid-related harm.
Sex, Gender, and Opioid Use
Sex-related factors affect how the body reacts to substances: how substances are metabolized, what amount causes intoxication, their effects on the brain, and the development of tolerance, dependence, or a disorder. Female and male bodies have different genetic and physiological characteristics that affect these processes.
Gender-related factors include the impacts of roles, norms, power imbalances, identity and institutional gender on men, women, and gender-diverse individuals. These affect risks and/or opportunities for use, impact of and exposure to marketing or exploitation, access to care and services, pressures to use, and the societal response to problematic use.
- Sex- and gender-related factors often interact to affect how substance use impacts fertility, pregnancy, breastfeeding, parenting, childcare, and sexual and intimate partner violence
Sex and gender influences on opioid use for women
Important gender differences relevant to the opioid crisis include:
- higher rates of prescription opioid use among women (64 percent of people who use opioid pain relievers are women; PACIRA, 2017),
- higher prevalence of many pain disorders, and
- higher prevalence of depression and anxiety disorders.
Women are more likely to be prescribed drugs that confer added risk when combined with opioids, such as anxiolytics.
- Women are more likely to misuse opioids after being prescribed them and are more likely than men to be admitted to hospital for intentional opioid overdose.
- Women progress from use of opioids to dependence more quickly than men and suffer more severe emotional and physical consequences of drug use than men.
- Data show that a majority of women living with addictions have suffered severe trauma, such as childhood sexual abuse.
Read the Guide: Women and Opioids from the partnership of Centre of Excellence for Women’s Health, Canada FASD Research Network and BC Women’s Hospital and Health Centre (BCCEWH, 2018)
Sex and Gender Influences on Opioid Use for Men
Masculine norms associated with substance use among boys and men are due in part to riskier forms of substance use by men. For example, men are more likely to:
- escalate their opioid medication doses,
- ingest opioid medications non-orally, and
- obtain prescription opioids via an illegitimate source.
Gendered patterns associated with masculinity, such as using alone, risk taking, and not seeking help are related to higher overdose deaths for men.
Compared to other types of substance use, both women and men who are addicted to prescription opioids are more likely to report a traumatic event and report higher rates of childhood trauma.
Gendered Influences on Opioid Use for Transgender Individuals

- Transgender individuals experience high rates of gender-based discrimination and violence, which are likely to influence use and problematic use.
- Girouard et al. (2019) in a commentary noted that little is known about the specific burden of the opioid crisis on lesbian, gay, bisexual, transgender, and queer (LGBTQ) persons.
- These authors recommend using a trauma-informed approach to care.
This workbook will help in integrating sex-and gender-informed evidence into practice.

Further Reading
 For those interested in sex-, gender-, and equity-based analysis in the substance use field, a primer from the Canadian Centre on Substance Use and Addiction will help to work through the steps. Sex, Gender and Equity Analyses [Report]
For those interested in sex-, gender-, and equity-based analysis in the substance use field, a primer from the Canadian Centre on Substance Use and Addiction will help to work through the steps. Sex, Gender and Equity Analyses [Report]
Racism and Opioid Use Disorders
- In 2012, the federal government enacted Bill C-10 (the Safe Street and Community Act) as part of the government’s national anti-drug strategy. One result was a police focus on Black communities and Black men and boys in particular, which resulted in a pattern of racialized criminalization and disproportionate incarceration.
- Indigenous men and women are also disproportionately incarcerated, which results in damaged individual and family lives, weakened communities, and intergenerational impacts.
- The pejorative associations of Black people and Indigenous people with crime have intensified levels of stigma and racism that have existed for decades.
- A critical discourse analysis of publications by the Canadian news media highlights the differences in media coverage of persons affected by opioid overdose with the most common image being of a young, white victim, outpacing reports of indigenous victims 30 to 1 (Johnston, 2020).
- The author reminds us that those who are given platform to speak are most often white, and rarely indigenous (p141).
- Diminished self-esteem, discrimination and internalized stigma are health risk factors borne by Black and Indigenous persons, placing them at higher risk for opioid use as a coping mechanism.
Colonialism, Structural Violence, and Trauma
For First Nations, colonization resulted in the loss of their culture, land, and language. The far-reaching intergenerational trauma is still experienced by many Indigenous people today, and it affects their health and well-being, including their substance use.
Read about Canada’s first peoples and the impact of colonialism in the Truth and Reconciliation Commission of Canada Report What we have learned: Principles of truth and reconciliation.
Trauma related to colonialism, residential schooling, family dislocation, and cultural genocide has resulted in communities struggling with:
- high rates of unemployment and poverty,
- low levels of education,
- inadequate housing,
- a disproportionate number of children in child protective services,
- addiction, and
- limited access to health care and social services.
Protective factors such as kinship systems, culture, and community have been removed or damaged by historical factors that include:
- the loss of language and connectedness to the land,
- lost rights to reserve housing for women who marry out,
- child removals,
- residential school abuses,
- systemic racism and sexism,
- environmental destruction, and
- cultural, spiritual, emotional, and mental disconnectedness.
Colonialism continues to impact Indigenous Peoples disproportionally in the form of addiction. In British Columbia, for example:

- The mortality rate for Indigenous people who use drugs is five times as high as for other drug users.
- Despite representing just 2.6 percent of the total population, Indigenous Peoples account for 10 percent of overdose deaths.
- Indigenous women are eight times as likely to have a nonfatal overdose and five times as likely to have a fatal overdose as non-Indigenous women.
The 2008–2010 First Nations Regional Health Survey revealed that of Indigenous people aged 18 and older living on-reserve or in northern First Nations communities, 4.7 percent reported past-year use of illegal (heroin) or prescription opioids (including morphine, methadone, and codeine) without a prescription, and 5.7 percent reported non-prescribed use of sedatives or sleeping pills, including diazepam and oxazepam.
It is critical to understand the impact and relationship between colonialism, racism and determinants of health and the risks opioid-related harm.
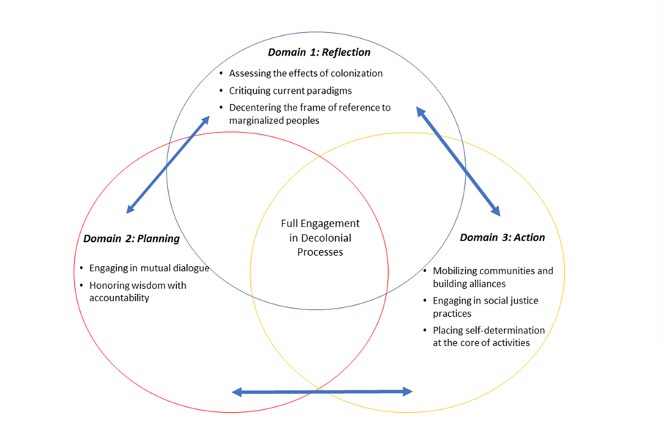
Decolonization is complementary to a trauma-informed approach where providers consistently question common and conventional knowledge and systems and partner with indigenous persons to redesign healthcare at all levels (Chandananbhumma & Narassimhan, 2020).
Chandananbhumma & Narassimhan (2020) propose a framework (Figure 1.) that includes three overlapping domains for use in decolonizing health promotion.
Figure 1. Applied decolonial framework for health promotion
Questions
How might an understanding of sex-related factors be applied in screening and assessment?
Consider sex-specific aspects such as anatomy, physiology, hormones, and brain responses of female and male bodies.
Feedback
Recognize that bodies differ in responding to substances: amounts, types, impact, tolerance, telescoping, addiction, and disorders, as well as to therapeutic drugs.
How might an understanding of gender-related factors, for women, men, and gender-diverse individuals, be applied in screening and assessment?
Consider roles, opportunities, norms, power, identity, interpersonal violence, impact of marketing and access to care.
Feedback
Recognize that sexism and gender-based violence affect interpersonal dynamics between people and their partners, helpers, and systems.
What aspect of the screening for opioid use can change knowing the historical and societal impact of racism, sexism, and colonialism?
Consider the intersecting impacts of racism, colonialism, sexism, and stigma on marginalizing Canadians such as Black people and Indigenous groups.
Feedback
Recognize the impact of social determinants of health and minority group status on access to care, response to health and social service providers, and trust of professionals.
References
Centre of Excellence for Women's Health. (2019). Sex, gender and women's use of opioids. http://bccewh.bc.ca/wp-content/uploads/2018/02/TGSInfoSheet-SexGenderOpioids021318.pdf
Centre of Excellence for Women's Health. (2020). Sex, gender and opioids. http://bccewh.bc.ca/wp-content/uploads/2020/05/CEWH-02-IGH-Handout_Opioids.pdf
Chandanabhumma, P.P., Narasimhan, S., 2020. Towards health equity and social justice: an applied framework of decolonization in health promotion. Health Promotion International 35, 831–840.
Greaves, L., Poole, N., Brabete, A. C., Hemsing, N., Stinson, J., & Wolfson, L. (2020). Integrating sex and gender informed evidence into your practices: Ten key questions on sex, gender. http://bccewh.bc.ca/wp-content/uploads/2020/05/CEWH-02-IGH-Handbook-Web.pdf
Girouard, M. P., Goldhammer, H., & Keuroghlian, A. S. (2019). Understanding and treating opioid use disorders in lesbian, gay, bisexual, transgender, and queer populations. Substance Abuse, 40(3), 335–339. https://doi.org/10.1080/08897077.2018.1544963
Johnston, G., 2020. The Kids Are All White: Examining Race and Representation in News Media Coverage of Opioid Overdose Deaths in Canada. Sociological Inquiry 90, 123–146.
Mazure, C.M., Fiellin, D.A., 2018. Women and opioids: something different is happening here. The Lancet 392, 9–11.
Nathoo, T., Poole, N., Wolfson, L., Schmidt, R., Hemsing, N., & Gelb, K. (2018). Doorways to conversation: Brief intervention on substance use with girls and women. http://bccewh.bc.ca/wp-content/uploads/2018/06/Doorways_ENGLISH_July-18-2018_online-version.pdf
PACIRA. (2017). United States for non-dependence: An analysis of the impact of opioid overprescribing in America. https://www.planagainstpain.com/wp-content/uploads/2017/09/PlanAgainstPain_USND.pdf
Poole, N., & Greaves, L. (2020). Sex, gender and equity analyses. Canadian Centre on Substance Use and Addiction. https://www.ccsa.ca/sex-and-gender-based-analysis
Regitz‐Zagrosek, V. (2012). Sex and gender differences in health: Science & Society Series on Sex and Science. EMBO Reports, 13(7), 596–603.
Schmidt, R., Poole, N., Greaves, L., & Hemsing, N. (2018). New terrain: Tools to integrate trauma and gender informed responses into substance use practice and policy. http://bccewh.bc.ca/wp-content/uploads/2018/06/NewTerrain_FinalOnlinePDF.pdf
Schmidt, R. A., Wolfson, L., Stinson, J., Poole, N., & Greaves, L. (2019). Mothering and opioids: Addressing stigma and acting collaboratively. http://bccewh.bc.ca/wp-content/uploads/2019/11/CEWH-03-MO-Toolkit_WEB_Update-F.pdf